Abstract

Only 25-30% of patients with Thalassemia major (TM) will have a suitable HLA-matched sibling donor for an allogeneic SCT. In the absence of a HLA-matched sibling, an extended donor search within the family may yield a suitable donor, especially in societies with a high prevalence of consanguinity. We have previously reported inferior outcomes in patients who had a transplant from a non-sibling family donor. One of the criticisms of this was the issue of low resolution typing, which may have adversely impacted outcomes in some patients. We interrogated this data further to assess whether the poorer outcomes held up to scrutiny with the availability of high resolution HLA typing. Towards this we undertook a retrospective case-control study, adjusting controls for age and Lucarelli risk group (common confounders for clinical outcomes post-transplant in TM) with a 4:1 ratio of controls to cases.
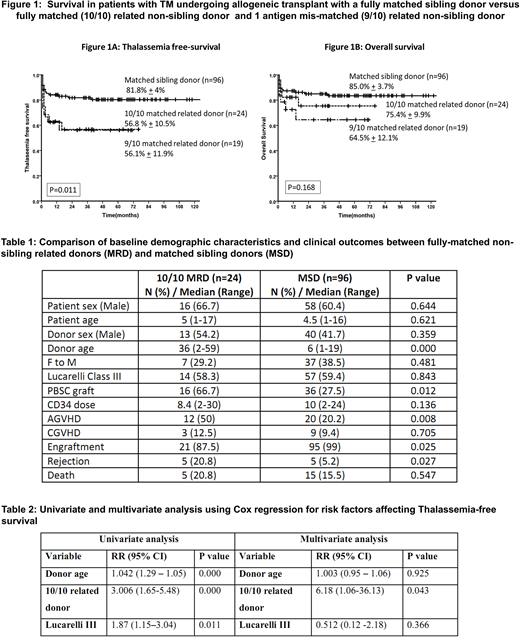
All consecutive patients with TM who had a stem cell transplant between the time periods 2007-2017, were included in this retrospective analysis. A total of 371 transplants were done with 281 matched sibling donor, 58 related donors (32 fully matched and 26 with 1-2 antigen mismatch), and 32 MUD donors (24 fully matched (10/10) and 8 with 1-antigen mismatch (9/10)).
Subsequent to 2012, high resolution typing was done for all non-sibling related family donors. Of the 58 related donors, high resolution typing was available in 45, with twenty four 10/10 donors, nineteen 9/10 donors and two 8/10 donors. Further analysis was done in this sub-group (excluding the 8/10 donors), with rejection and death being considered as events. A control group from the fully matched sibling donor cohort was generated randomly after adjusting for age and Lucarelli Class.
All patients received a myeloablative conditioning regimen (Busulphan/Treosulfan based). In-vivo T-cell depletion was done in 11 (45.8%) of matched related transplants and 54 (56.2%) of matched sibling donor transplants (P=0.359). A PBSC graft was used in 16 (66.7%) of matched related donor transplants compared with 36 (27.5%) of matched sibling donor transplants (P=0.012). There was no difference in the median CD34 cell dose achieved in both groups (Table 1). Table 1 shows baseline characteristics, transplant details and outcomes in the 10/10 matched related donors and fully matched sibling donor groups. Table 2 shows univariate and multivariate analysis for risk factors adversely affecting Thalassemia-free survival (TFS) using Cox regression analysis. The 2-year TFS in the 10/10 matched related donor group, 9/10 matched related donor group and fully matched sibling donor group was 56.8%±10.5%, 56.1%±11.9% and 81.8%±4% respectively (P=0.011) (Figure 1A). The 2-year overall survival (OS) in the 10/10 matched related donor group and 9/10 matched related donor group and the fully matched sibling donor group was 75.4%±9.9%, 64.5%±12.1% and 85.0%±3.7% respectively (P=0.168) (Figure 1B).
This data on allogeneic transplants confirms our previous observations that there is a higher risk of graft rejection when the donor is a non-sibling related donor, even if fully matched on high-resolution typing (OR 4.8 ; 95% CI=1.3-18.2 : P=0.02). Transplant physicians must be aware this increased risk and counsel families appropriately. Further modifications in conditioning regimens and GVHD prophylaxis could potentially help in improving these outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal